Bone Augmentation with Titanium mesh
- Dr. Tan Soon Teik
- Sep 11, 2015
- 3 min read

Risk Assessment
- Class 1 skeletal with enough lip support with flangeless denture
- Moderate gingiva biotype thickness
- Moderate gingiva biotype display
- Squarish existing denture teeth (to conform to the existing mould of tooth shape)
- Horizontal ridge resorption in general with vertical loss at 22 region
- Adjacent interproximal crestal bone height reasonable.
No perio pocketing
Treatment Plan
- 2 stage surgical approach
- Horizontal and vertical augmentation with Ti-mesh using Allogenic particulate graft
- 2 Implants to be placed for screw retained fixed bridge
- Provisional bridge for creating emergence profile
- Final restoration

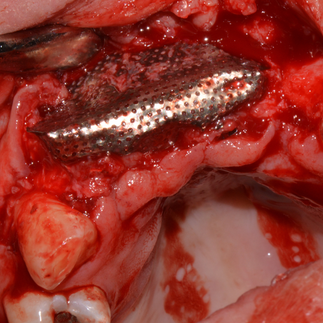
Thin crestal ridge with apical concavity
Marrow penetration and adaptation with trimming of Titanium mesh
Allogenic particulate graft placed.
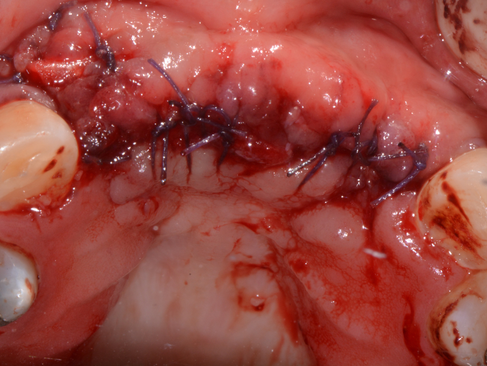
Periosteal splitting done for tension free primary closure.
Tension free primary closure with double sling suture.
Horizontal mattress suture and simple interrupted suture.
3 Months review: Soft tissue thinning on the right quadrant & vertical height on the left side sufficient
5 Months review: Dehiscence of soft tissue. Decision made to remove Ti- mesh and place implants.
Ti-mesh exposed.
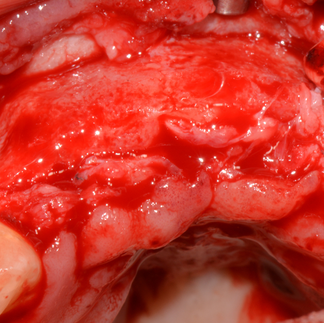
Thin pseudo-periosteum covering newly regenerated bone present under Ti-mesh
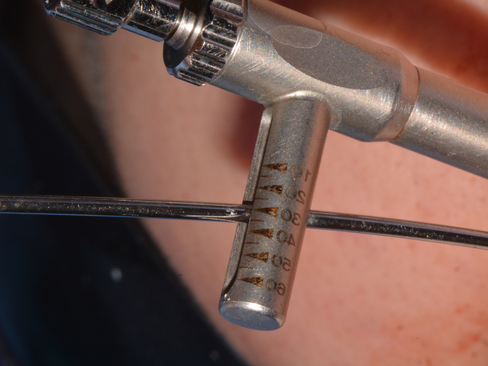
Implant osteotomy with the help of surgical guide and parallel pins

Ridge width at crestal still slightly insufficient
Insertion torque right vs left are 30Ncm and 25Ncm respectively

Additional GBR was planned and to cover dehisence site collagen membrane. Periosteal incision was made.
GBR performed with collagen membrane and particulate allogenic graft (Regenoss)
Tension free primary closure done.

Pre-operative Radiograph
2 Weeks review after Implant placement and GBR
1 Month review after Implant placement and GBR
Healing after 10 weeks

Healing abutment placement
3 Weeks after healing abutment placed
Impression to fabricated provisional bridge
Prior provisional placement thick soft tissue label to Implants
Screw retained provisional bridge to form soft tissue emergence profile to take final impression in 2-3 months after soft tissue achieves pleasing emergence profile.
Discussion
-Undoubtedly, ti mesh can predictably augment ridge both vertically and horizontally.
- But this method has high soft tissue complication (22.78%), meaning almost 1 out of 5 cases will encounter dehiscence.
- It was reported that ti mesh exposure is probably attributable to its low flexibility (watzinger et al 2000) or the suturing technique used (pinho et al 2006).
- Rakhmatia et al 2014 did a microcomputed tomography & histomorphometric analysis on different titanium membranes with differenet thickness and pore sizes in rat calvarial defect model.
- The greatest bone volume gain was noticed on 100 micron thick membranes with large pores, but with lower mineral density
- Soft tissue ingrowth on that group was increased at 4 weeks but decreased by 8 weeks to a level not statistically significant to other ti membrane groups
- They concluded that ti mesh thickness affect the bone volume gained and the mesh porosity played an essential part in bone regeneration especially at the initial healing period as vascularity of the soft tissue was not disturbed.
- Torres et al 2010 did a human randomized controlled trial to evaluate the use of platelet-rich-plasma (prp) as a method to prevent ti mesh exposure in alveolar ridge augmentation with anorganic bovine bone.
- They found that the control group without PRP suffered 28.5% of mesh exposure whereas no exposure was found in the PRP group (statistically significant).
- Radiographic analysis also showed higher bone gain in the PRP group. They concluded that due to the improve soft tissue healing capacity by PRP, the mesh and graft material were protected under the soft tissue without any dehiscence.
- Ti-mesh exposure provoked significant bone loss but in most cases did not affect the subsequent placement of implants our text here to convert case
Further Suggestion
- Additional growth factor to prevent soft tissue complication
- More randomized controlled trials to determine the ideal thickness and porosity of titanium mesh to minimize the thickness of pseudo-periosteum formed underneath the mesh
- Improvement in the mesh material for better adaptation and manipulation
- Better surgical protocol - 3d printed mesh or pre-surgical adaptation on stereolythic model
- Improve surgical instrument to ease soft tissue manipulation
- Better tension free closure and suturing technique
Conclusion
- Titanium mesh augmentation is predictable to gain both horizontal and vertical bone dimension
- Soft tissue is the issue





































































Comments