Class III M Fixation with Sinus Crestal Elevation and GBR with a Ti mesh
- Dr. YoungKu Heo

- Jun 29, 2017
- 2 min read
The maxillary left 2nd premolar (#25) was extracted due to severe bone loss and mobility. After 3 weeks of soft tissue healing, 3 implants were placed at the #25, 26, 27 sites. Crestal sinus grafting was performed for all three sites with the S-reamer (SCA tech.) Following the implant placement, large bony defects were noted around the #25 & 27 fixtures (Class III M fixation). The gaps between fixtures and the walls of the bony defects were filled with allogenic graft material. Following the bone packing, a titanium mesh was covered over the graft site, and fixed with suture material. A titanium membrane with a collagen membrane cover is preferred for the graft due to its excellent space maintenance. After 10 weeks, the titanium mesh was removed, and the graft site revealed bone overgrowing.Healing abutments were connected.
SITUATION

A 58-year-old male, good general health despite 20 years of smoking.
Pre-op panorama: Bilateral partial edentulism on the maxilla. Both posterior regions require sinus augmentation for implant placement. Severe bone loss and PDL space widening around the maxillary left 2nd premolar (#25). The extraction socket of the 2nd molar (#27) was not completely healed.

Soft tissue healing three weeks post-extraction.

Bony defects at the extraction sites of 2nd premolar and 2nd molar.

Crestal approach for sinus lifting and grafting with the SCA reamer.

Crestal approach for sinus lifting and grafting with the SCA reamer.

Crestal approach for sinus lifting and grafting with the SCA reamer.

Three implants placed at the sites of #25, 26, 27. The threads of the #25, 27 implants are exposed due to the size of the bony defect.

FDBA graft packed over the implants and defects.

A titanium membrane was placed over the graft.

Titanium membranes are preferred to resorbable membranes in terms of space maintenance.

Interrupted suture with supramid 4-0.

Post-op panorama.
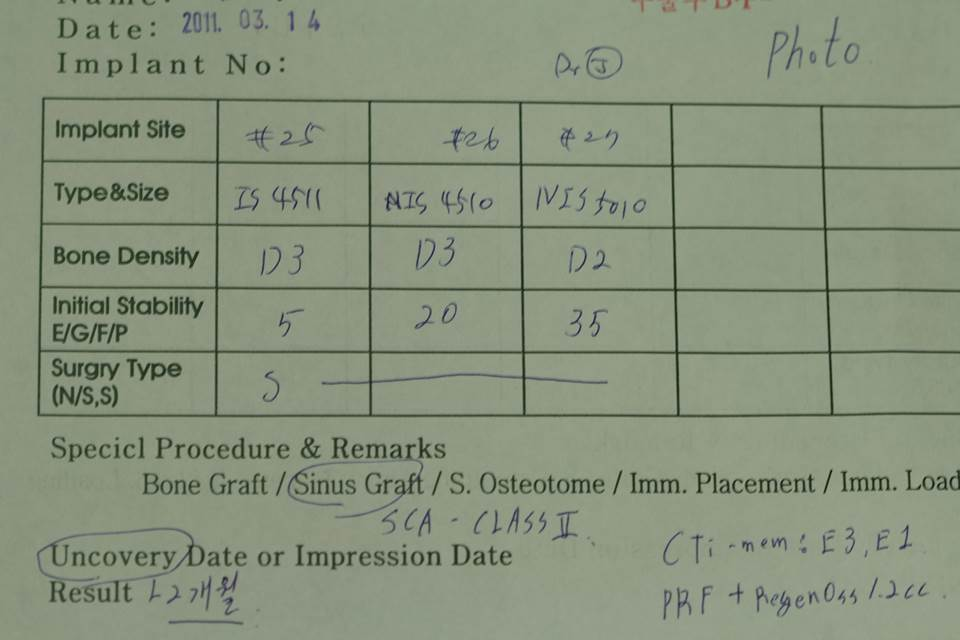
As shown in the chart, the initial stability for #25 was low (approx. 5 Ncm), compared to 20 Ncm for #26 and 35 Ncm for #27 respectively.

Soft tissue healing at 2nd surgery.

Removal of titanium membrane after 10 weeks.

Note the excellent bone formation underneath the titanium membrane.

The implants were uncovered by removing the excess bone formed on top of the implants.

Unique flap design to maximize the keratinized gingiva.

The final prosthesis on the left side will be fabricated after the grafted bone matures.

Soft tissue was healed around healing abutment after 2nd surgery.

Monolithic zirconia restorations were fabricated for final prosthesis.

Stock abutments were milled to fabricate cement-retained prosthesis.
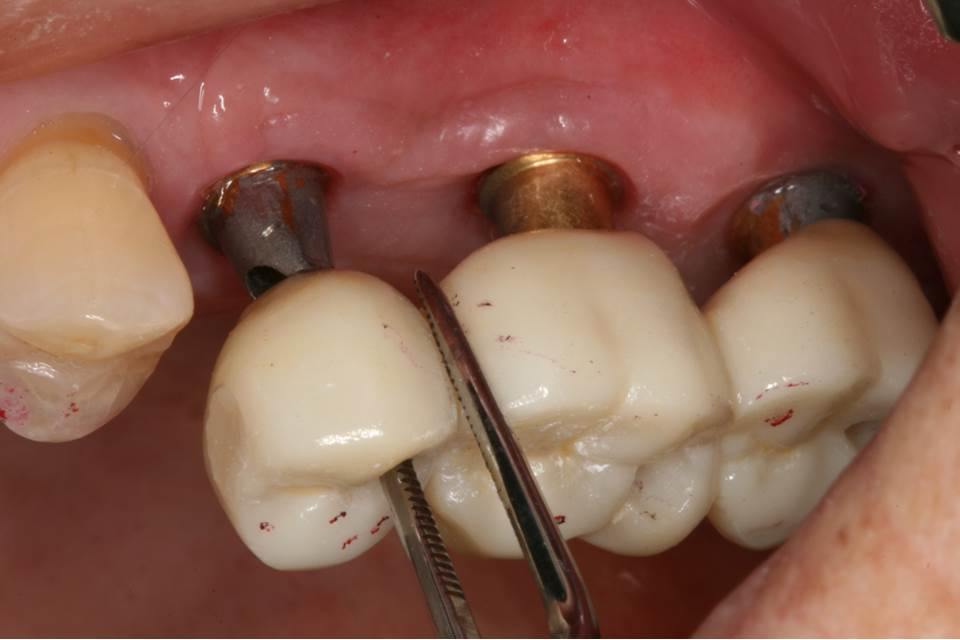
The final prosthesis (splinted monolithic zirconia crowns) was delivered after contact and occlusal adjustments.

The final prosthesis (splinted monolithic zirconia crowns) was delivered after contact and occlusal adjustments.

Occlusal access holes (for SCRP prosthesis) were prepared at the fossa areas.

The fit of the prosthesis was verified on periapical x-ray.

After final cementation with permanent resin cement and removal of the excess cement by removing the whole prosthesis.

3-year follow-up panorama.

5-year follow-up panorama.

6-year follow-up panorama.



Comments