Aesthetic Rehabilitation in the Anterior Zone. Implant Placement and Inmediate Loading: Alveolar and Soft Tissue Reconstruction
- GAO
- Nov 14, 2025
- 4 min read

Dr. Edgar Paul Gonzalez
(Santiago, Dominican Republic)
Case Summary 🔎
Patient Information
Male, 31 years old
Systemic condition: ASA I
Medical history (PMH): Non-contributory
Dental history (PDH): Localized vestibular bone deficiency in the anterior region.
Diagnosis: Moderate horizontal bone defect with thin gingival biotype and partial vestibular support loss.
Clinical findings: Alveolar contour collapse, marginal exposure of the vestibular tissue, indicating the need for a combined surgical–restorative approach.

Descriptions
A 31-year-old male presented with a horizontal bone defect in the anterior maxillary region, compromising vestibular contour and soft-tissue stability.
The treatment goal was to achieve an immediate aesthetic rehabilitation through guided implant placement, accompanied by bone regeneration and soft-tissue thickening to ensure long-term functional and aesthetic stability.
The case was digitally planned following the principles of the EZP – Esthetic Zone Implant Placement Protocol, emphasizing prosthetically driven 3D positioning and creating of the emergence profile.
Treatment Plan
1. Immediate placement of a Neobiotech IS-II Active 3.5 X 11.5 mm implant in prosthetically driven three-dimensional position (tooth #21)
2. Horizontal guided bone regeneration (GBR) using particulate autograft collected by scraping from the external oblique ridge.
3. Supplementary filling with particulate allograft to preserve the vestibular cortical plate.
4. Connective tissue graft (CTG) obtained by de-epithelialization of a free gingival graft (no flap elevation) for soft-tissue thickening and stabilization.
5. Immediate provisional restoration to shape the emergence profile and preserve the gingival architecture.
Case Presentation
Patient Information
Male, 31 years old
Systemic condition: ASA I
Medical history (PMH): Non-contributory
Dental history (PDH): Localized vestibular bone deficiency in the anterior region.


Diagnosis
Moderate horizontal bone defect with thin gingival biotype and partial vestibular support loss.
Clinical findings
Alveolar contour collapse, marginal exposure of the vestibular tissue, indicating the need for a combined surgical–restorative approach.
Treatment Plan
Immediate placement of a Neobiotech IS-II Active 3.5 X 11.5 mm implant in prosthetically driven three-dimensional position (tooth #21)
Horizontal guided bone regeneration (GBR) using particulate autograft collected by scraping from the external oblique ridge.
Supplementary filling with particulate allograft to preserve the vestibular cortical plate.
Connective tissue graft (CTG) obtained by de-epithelialization of a free gingival graft (no flap elevation) for soft-tissue thickening and stabilization.
Immediate provisional restoration to shape the emergence profile and preserve the gingival architecture.

Case Presentation
1️⃣Pre-op
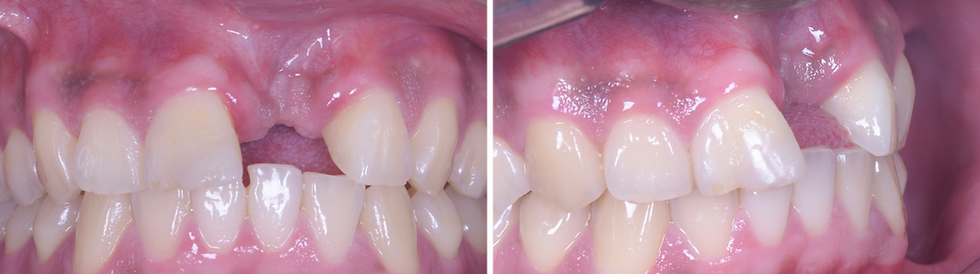
Pre-operative frontal view showing vestibular bone deficiency and gingival collapse
Pre-operative Examination (Panoramic View of CT scan)
Initial radiograph revealing localized horizontal bone loss.



After seating the surgical guide and completing the initial to final drilling sequence, the guide was removed to verify bone exposure and confirm the planned osteotomy trajectory.


Guided placement of Neobiotech IS-II Active 3.5 × 11.5 mm implant (insertion torque = 60 Ncm).
Implant positioned in its final three-dimensional, prosthetically driven location. Note the vestibular fenestration observed at the time of placement.
Immediate screw-retained provisional crown shaping the emergence profile.


Harvesting of particulate autogenous bone by scraping the external oblique ridge.
Placement of the autograft in the vestibular zone for horizontal ridge augmentation. Note the fixation of the membrane in the vestibular area using tacks to ensure graft stability.

Placement of demineralized particulate allograft over the vestibular surface to enhance ridge volume and support cortical preservation.
Membrane secured in position, providing stable coverage of the grafted area and ensuring proper containment of the regenerative materials.

Connective tissue graft harvested from the palatal area, prepared for placement to increase mucosal thickness and enhance soft-tissue stability.
Connective tissue graft sutured in position

Pre- and immediate postoperative intraoral views demonstrating accurate 3D implant positioning and graft stability.

1️⃣Pre-op
Pre-operative frontal view showing vestibular bone deficiency and gingival collapse.
3D CT and intraoral scans were used to virtually plan the prosthetically driven implant position, angulation, and depth.
Initial radiograph revealing localized horizontal bone loss.



Surgical guide positioning followed by sequential drilling from the initial pilot drill to the final drill.
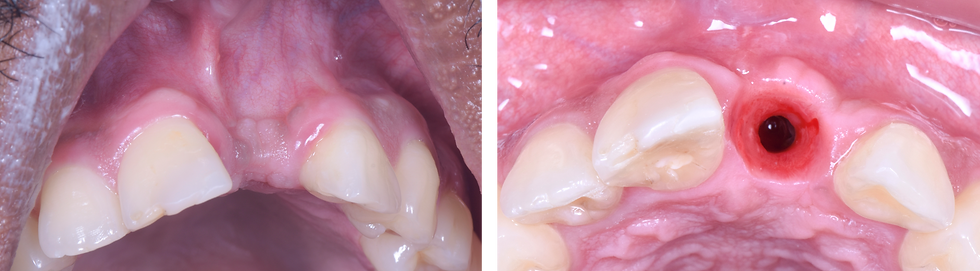
Implant positioned in its final three-dimensional, prosthetically driven location. Note the vestibular fenestration observed at the time of placement.
2️⃣ Surgery


Implant positioned in its final three-dimensional, prosthetically driven location. Note the vestibular fenestration observed at the time of placement.
In D333 bone quality the IS-III 3.5×11.5 implant was placed with excellent primary stability, achieving an insertion torque of 60 Ncm.
Followed by immediate screw-retained provisionalization to shape the emergence profile.

Harvesting of particulate autogenous bone by scraping the external oblique ridge
Placement of the autograft in the vestibular zone for horizontal ridge augmentation. Note the fixation of the membrane in the vestibular area using tacks to ensure graft stability.

Placement of demineralized particulate allograft over the vestibular surface to enhance ridge volume and support cortical preservation.
Membrane secured in position, providing stable coverage of the grafted area and ensuring proper containment of the regenerative materials.

Connective tissue graft harvested from the palatal area, prepared for placement to increase mucosal thickness and enhance soft-tissue stability.
Connective tissue graft sutured in position.

The postoperative image and radiograph display the implant placement and the bone and soft-tissue grafts in comparison with the preoperative view.

3️⃣Result
Clinical views at 7 days and 15 days postoperative

Initial Situation and Six-Month Postoperative View
Occlusal view at the 6-month follow-up showing healthy peri-implant tissues and a well-defined, stable emergence profile.




Comments